Thyroid Eye Disease
Thyroid eye disease is a disorder of the immune system. It is not understood why our body’s protective defenses begin to attack the body’s own tissues. In thyroid eye disease the tissue around the eye is attacked by inflammatory cells and the result is inflammation, swelling, and bulging of the eye.
Thyroid disease and thyroid eye disease both come from the immune system attacking healthy tissue. We now know one disease does not directly cause the other. The immune system may attack both the thyroid and the tissue around the eye. The timing and severity of these two diseases is variable depending on the individual. Sometimes the thyroid can be low, sometimes it can be high, and rarely there will be no thyroid abnormality but the eyes will have symptoms of thyroid eye disease.
Common symptoms of thyroid eye disease include swelling around the eyes, bulging of the eyes, irritation, redness, and a pressure sensation associated with headache. There can be pain with eye movement and/or restriction of eye movements causing double vision. If the inflammation involves the muscles, or if the swelling is severe enough, the pressure in the orbit (eye socket) can become extremely high. This can cause compression of the optic nerve, resulting in progressive loss of vision, and possibly blindness if the condition is not treated promptly.
There are two phases of thyroid eye disease. The first phase is the inflammatory (active) phase, which typically lasts six months to two years. The second phase is the stable (chronic) phase when active inflammation is quiet. Many patients will be left with some degree of protrusion of the eye, eyelid retraction, or double vision that may require additional treatment.
Chronic eye exposure from protrusion or lid retraction can lead to severe drying of the eye and corneal scarring. Double vision can be severe and disabling. Depending on the severity of the thyroid eye disease, all patients should be followed closely by an expert.
Treatments
For many, the discomfort from thyroid eye disease can be treated with topical lubricants, wrap-around tinted glasses, sleeping with eye shields, or elevating the head of the bed at night.
When there is active inflammation, certain treatment modalities have been tried including steroids, anti-inflammatory medicines, and radiation. Promising new drugs and other treatments may improve the treatment of active thyroid eye disease. Teprotumumab is a newer medication that is sometimes used to treat thyroid eye disease.
Usually, surgery is not performed until the disease becomes stable. If there is compressive optic neuropathy or significant dryness, sometimes surgery will be performed during the active phase of the disease.
The function and appearance of the eyes can usually be improved by reconstructive eyelid or orbital surgery. The particular surgical technique used will depend on the type and severity of the eye problems, but typically progresses in three stages. Not all patients with thyroid eye disease will require all of these treatments.
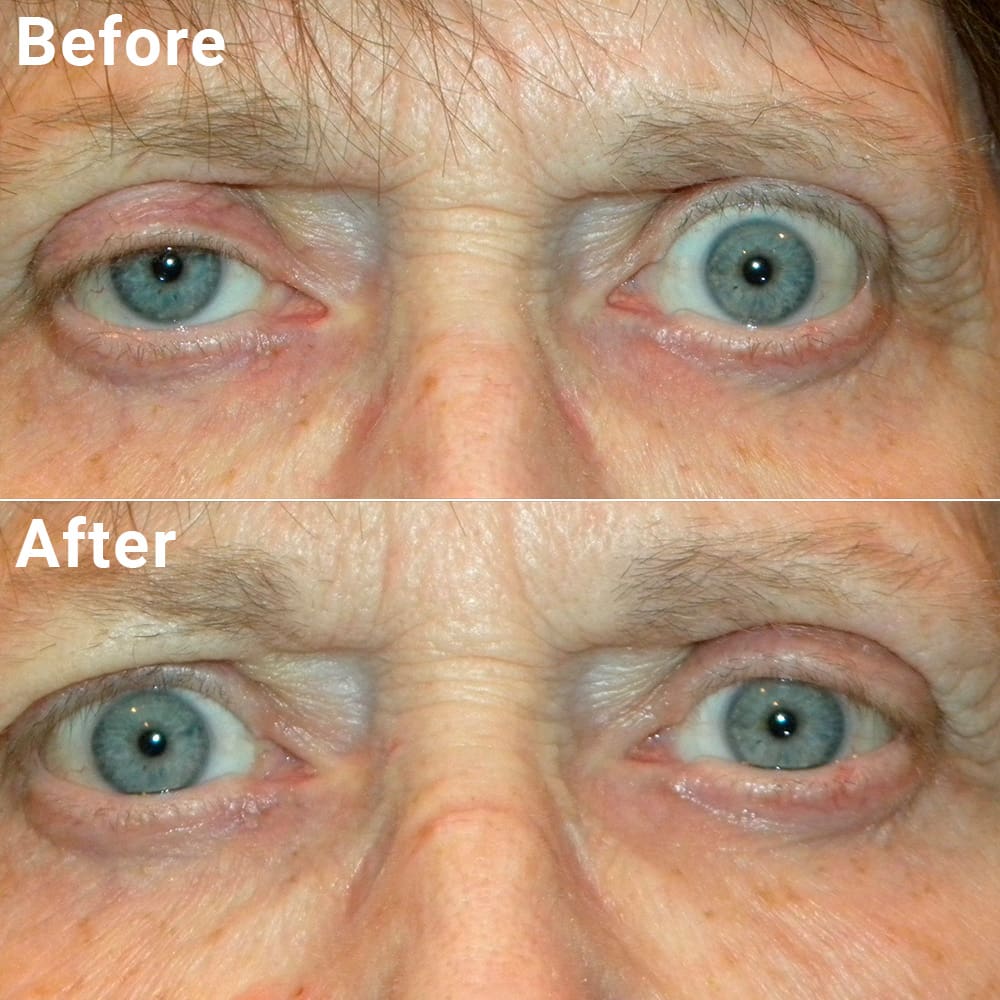
Stage one of surgery is orbital decompression (removing part of the bony orbit and fat behind the eye to relieve pressure in the eye socket). This can prevent damage to the optic nerve and allow the eye to move back into a more normal position in the eye socket. This is usually performed by an oculofacial plastic surgeon.
Stage two is eye muscle surgery to correct misalignment of the eyes and double vision. This is achieved by repositioning the enlarged muscles that control eye movement. This is usually performed by a strabismus specialist, often a pediatric ophthalmologist.
Stage three is eyelid surgery to adjust the position of retracted lids in order to improve eyelid closure and restore eyelid function. Removal of excessive fat from the eyelids can also improve their appearance. This is usually performed by an oculofacial plastic surgeon.
While it may not be possible to completely eliminate all of the consequences of thyroid eye disease, surgery to correct these conditions is generally successful in satisfactorily restoring function, comfort, and cosmetic appearance.
Risks and Complications
Bruising and/or swelling may be expected and will likely go away in one to two weeks. Bleeding, infection, anesthesia risks, and scarring are potential complications of the surgery, but fortunately uncommon. Be sure to tell your surgeon if you are on blood thinners as their use may put you at increased risk for bleeding complications.
Your surgeon cannot control all the variables that may impact your final result. The goal is always to improve a patient’s condition but no guarantees or promises can be made for a successful outcome in any surgical procedure. There is always a chance you will not be satisfied with your results and/or that you will need additional treatment. As with any medical decision, there may be other inherent risks or alternatives that should be discussed with your surgeon.